COBRA Audit Work Program
Auditing Compliance with COBRA Regulations
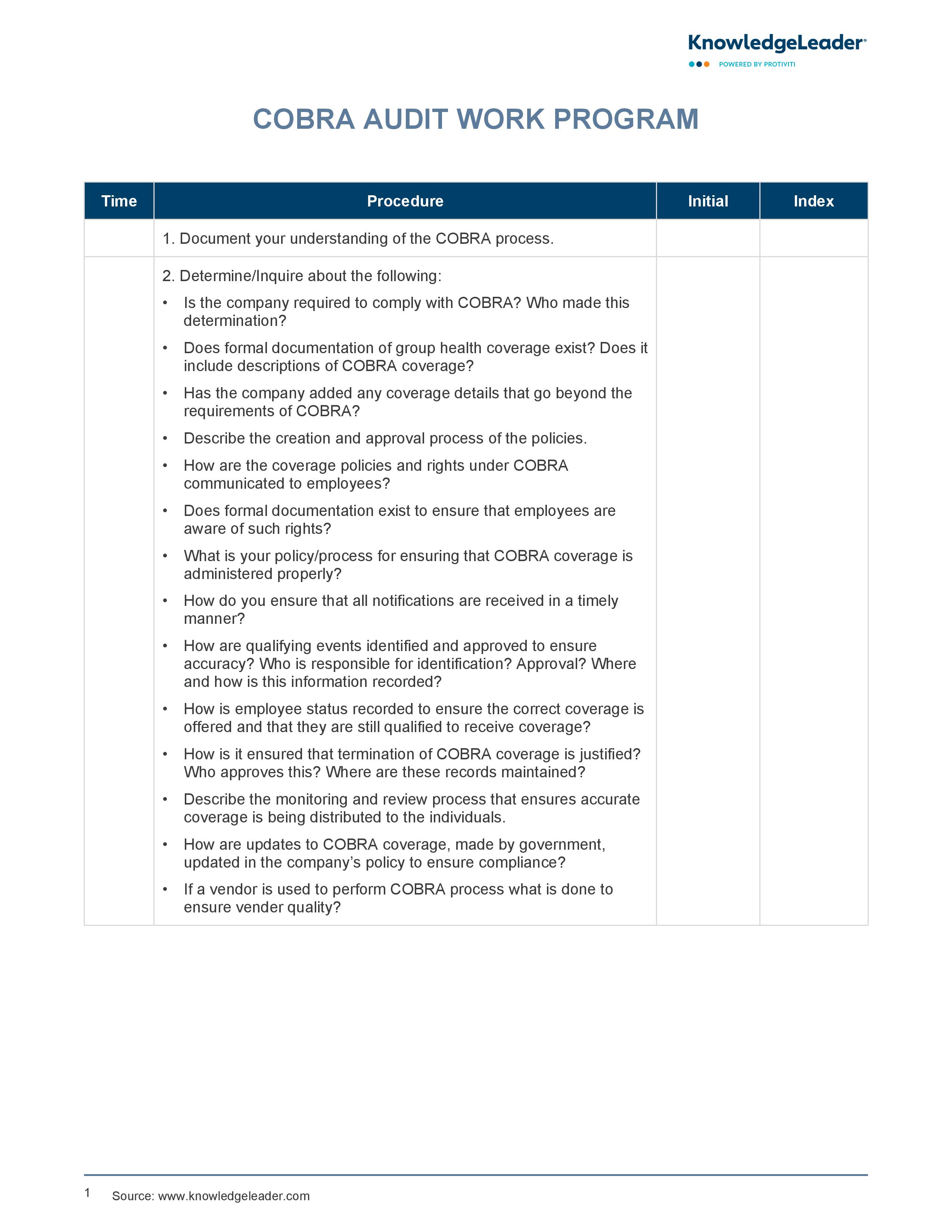
Our COBRA Audit Work Program can be used by companies to perform audits on their COBRA (Consolidated Omnibus Budget Reconciliation Act) compliance practices. This involves ensuring the company's adherence to mandated health insurance coverage for employees after job loss or other qualifying events. It includes a series of procedures on obtaining formal documentation of the company's health plan and COBRA policy, verifying vendor selection, checking communication of amendments and notices, and validating the identification of qualifying events.
The program also guides how to test approvals using an authorization matrix and advises on conducting interviews or surveys with employees currently receiving COBRA coverage. Moreover, it provides steps for reviewing records related to coverage terminations and ensures employee awareness about their rights under the group health plan and COBRA. Therefore, this document is crucial for companies in maintaining regulatory compliance, mitigating risk exposure related to health coverage provisions and fostering transparency within their workforce.
Sample auditing questions to consider include:
- Is the company required to comply with COBRA? Who made this determination?
- Does formal documentation of group health coverage exist? Does it include descriptions of COBRA coverage?
- Has the company added any coverage details that go beyond the requirements of COBRA?