Membership and Billing Audit Work Program
A Detailed Review of Membership & Billing Practices
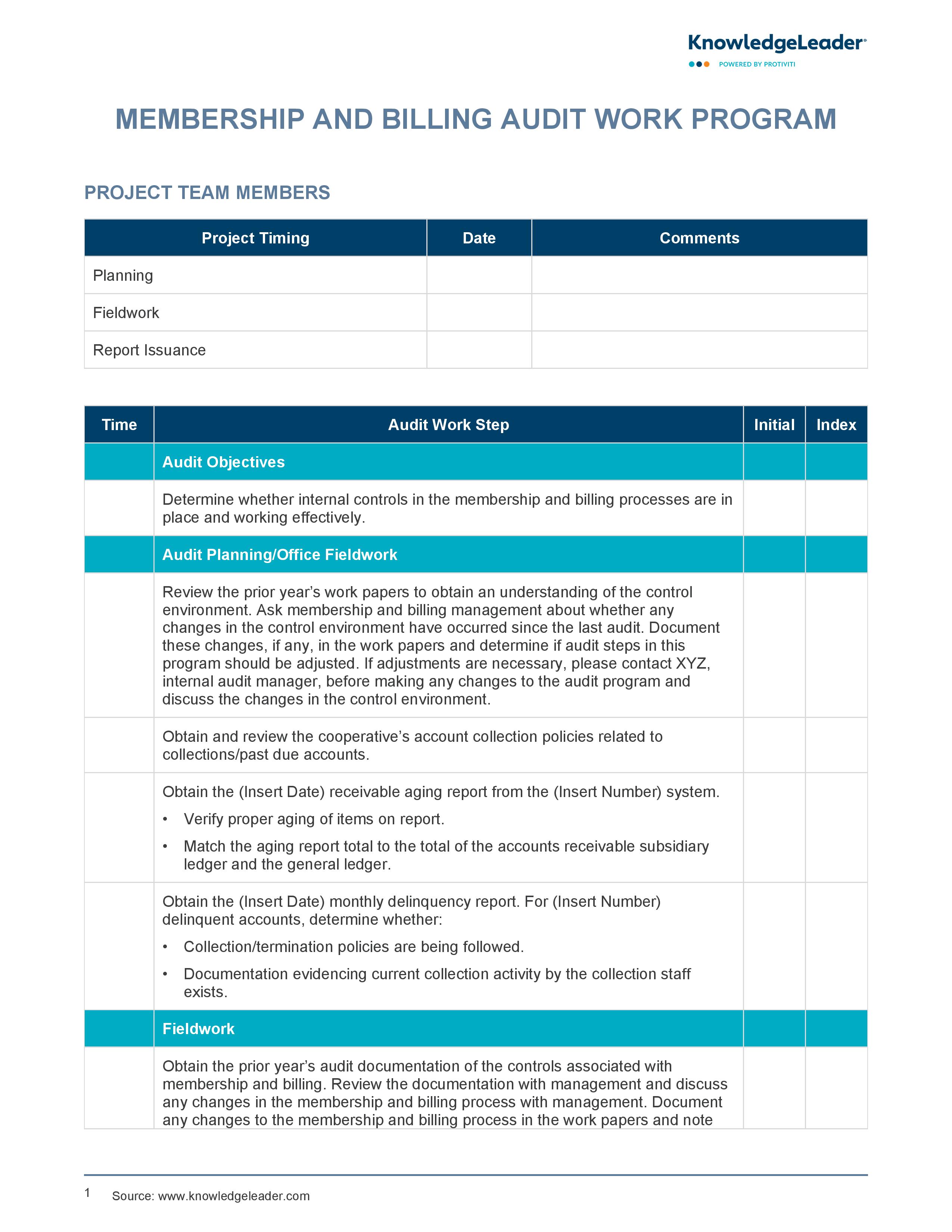
Our Membership and Billing Audit Work Program reviews the membership and billing process within a healthcare cooperative. The work program’s main objective is to determine whether internal controls in these areas are functioning effectively. The program includes a variety of audit steps, such as reviewing prior year's work papers, examining account collection policies, verifying receivable aging reports and assessing delinquency reports. It also involves detailed checks on member records, group contract rates, refunds, adjustments, credits, reconciliations and cash receipts.
The document provides a systematic and comprehensive approach to evaluate the accuracy, timeliness and appropriateness of transactions and processes. It helps in identifying any discrepancies, inefficiencies or weaknesses in the existing systems, enabling the organization to take corrective actions and improve its operations. This audit work program is a valuable tool for ensuring transparency, accountability and compliance in the membership and billing operations of an organization.
Best-practice audit work steps include:
- Asking about the process in place to monitor status changes
- Determining whether contracts were renewed timely
- Determining and documenting the cause for delay if the renewal rates were entered into the system after the expiration date
- Determining whether the contract includes an arbitration clause