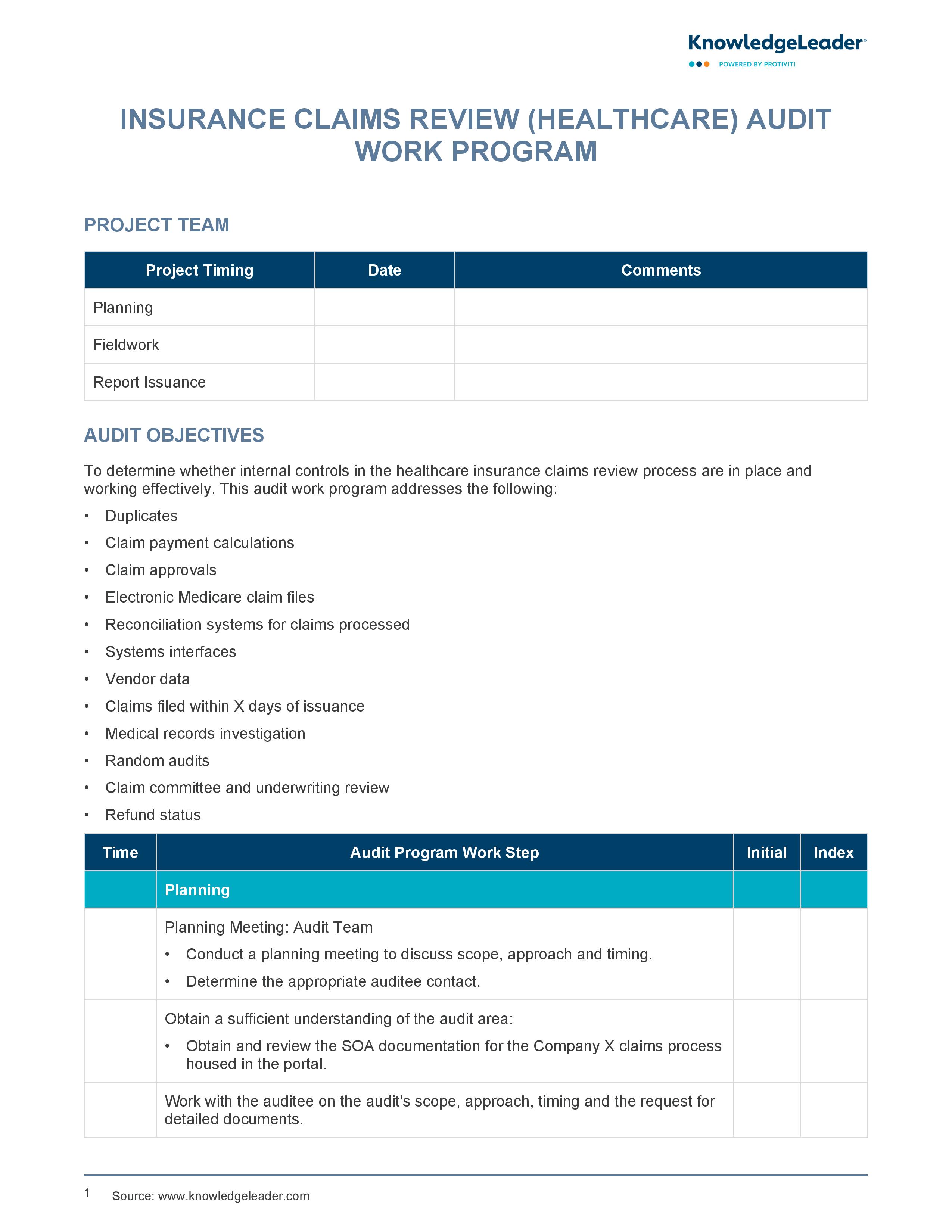
Insurance Claims Review (Healthcare) Audit Work Program
A Sample Work Program to Audit the Health Insurance Claims Review Process
Our Insurance Claims Review (Healthcare) Audit Work Program provides a framework for effectively evaluating the internal controls in the healthcare insurance claims review process. It covers a wide range of aspects including duplicates, claim payment calculations, claim approvals, electronic Medicare claim files, reconciliation systems for claims processed, systems interfaces, vendor data and more. The tool facilitates meticulous planning, fieldwork and report issuance phases, ensuring a thorough understanding of the audit area and promoting open communication with auditee contacts.
This document also includes comprehensive testing for potential duplicate claims, claim payment calculations and claim approvals. Additionally, it assists with reconciling different systems, validating intermediary files, and conducting various claim reviews, audits and investigations. Finally, it ensures a systematic report phase where findings are validated, draft reports are cleared with process owners, and final reports are issued incorporating management responses. Overall, this tool offers a robust approach to auditing the insurance claims review process in healthcare, enhancing the efficiency and effectiveness of the audit.
This audit work program addresses the following:
- Duplicates
- Claim payment calculations
- Claim approvals
- Electronic Medicare claim files